Depression Part II: Therapeutic Treatment Options
By Ari Goldstein, Ph.D.
According to Dr. Stephen Ildari, author of “The Depression Cure,” the human race is experiencing a global epidemic of depression because, “we were never designed for the sedentary, indoor, sleep-deprived, socially-isolated, fast-food-laden, frenetic pace of modern life.”
Ildari, an associate professor of clinical psychology at the University of Kansas, claims that depression is actually a form of the fight or flight response early humans developed when faced with physical dangers or predators. This condition enables the body to go through the intense physical activity required to escape a life threatening condition such as fire or an animal attack for hours or even days. However, Ildari postulates, “for many people throughout the Western world, the stress response goes on for weeks, months and even years at a time, and when it does that, it’s incredibly toxic.”
Following up on this theory, Ildari proposes that to prevent and permanently cure depression we should follow this six-step regime to create a lifestyle similar to that of depression–free, pre-historic hunter-gatherers:
-Take daily doses of 1,500 mg of omega-3 plus a multivitamin and 500 mg of Vitamin C
– Don’t dwell on negative thoughts – instead, participate in some sort of activity with others
– Exercise for 90 minutes per week
-Get 15 to 30 minutes of sunlight each morning in the summer and consider using a lightbox in the winter
– Be sociable – interact on a regular basis with other people
– Get 8 hours of sleep each night
Apparently, Ildari developed the six steps described above as an alternative to pharmaceutical therapy for depression that he regards as largely ineffective.
Where did taking drugs for depression begin anyway?
Humanity has actually been looking to “cure the blues” for Millennia. Whether it was drinking fermented beverages, smoking opium and hashish, or using stimulants like cocaine, the dream of finding an instant cure for sadness has been with us for a long, long time.
In the 1980’s pharmaceutical giant, Eli Lilly and Company introduced a new drug called Prozac to the public. Originally called Fluoxetine, the formula was intended and tested to treat high blood pressure and later obesity. When it failed to be effective in treating these conditions, it was given to a small group of people suffering from mild depression. Viola! Prozac seemed to cheer up those who were chronically sad and, perhaps just as importantly, it didn’t seem to have the same potential for dangerous side effects – addiction and overdosing – that were becoming associated with the anti-anxiety drug, Valium.
Prozac also benefited by coming along at a time when the rules were loosening for marketing pharmaceuticals. So Eli Lilly hired a branding company that scrapped “Fluoxetine” for “Prozac,” creating a name that starts with “Pro” to indicate a “positive” and “professional” outcome, followed by a “Z” suggesting strength and high technology, then ending with “ac” to convey “action.” The result of this marketing ploy was that by 2012, thirteen per cent of Americans were taking Prozac or some other antidepressant. All of these drugs generally fall into several different categories, each having its own advantages and weaknesses. Here’s a brief description and some examples of these medication types:
- Selective serotonin re-uptake inhibitors (SSRIs).
This group of drugs includes Prozac, Paxil, Zoloft, Celexa and Lexapro. They may have some side effects including upset stomach, jitteriness, insomnia and a decrease in sexual desire. Among the newest treatments for depression, SSRIs are reportedly safer than some prescriptions used in the past. The popularity of these drugs centers on their ability to increase serotonin levels in the brain. Studies done decades ago indicated depressed people have low serotonin levels and when these levels were raised, patients became more energetic and less sad.
- Serotonin and norepinephrine reuptake inhibitors (SNRIs).
These medications include Cymbalta, Effexor and Pristiq. Their side effects resemble those caused by SSRIs and, in large doses, can also cause dizziness and excessive sweating. They also work by raising the levels of serotonin as well as norepinephrine, another neurotransmitter in the brain.
- Norepinephrine and dopamine reuptake inhibitors (NDRIs).
Wellbutrin is an example of this category and works by increasing dopamine as well as norepinephrine in the brain. In contrast to SSRIs and SNRIs, NDRIs don’t seem to lessen sexual desire or activity but if taken in high doses may increase the risk of seizures.
- Tricyclic antidepressants (TCAs).
Used for years, TCAs are often as effective as the newer SSRIs and SRNIs but have more side effects such as low blood pressure, dry mouth, blurred vision, constipation, urinary retention, fast heartbeat and confusion. They can also cause weight gain and in older patients can cause memory problems and even hallucinations. Like the newer drugs, they work by increasing the amount of serotonin and/or norepinephrine in the brain.
- Monoamine oxidase inhibitors (MAOIs).
MAOIs, such a Parnate and Nardil, also increase serotonin levels but are generally prescribed only if other medications haven’t worked. This is because the side effects of MAOIs are more serious. These drugs also require a strict adherence to a limited diet in order to avoid potentially deadly interaction with certain foods and other medications. One of the newer MAOIs – Emsam – may have fewer of these complications and is designed to work as a skin patch instead of a pill.
- Atypical antidepressants.
Medications like Desyrel and Remeron are called atypical because they can’t be put into any existing antidepressant category. Since they act as sedatives, they are usually prescribed for nighttime use and may be given along with other antidepressants to relieve insomnia.
Finding the right medication can be half the battle.
Treating depression is often a case of trial and error to find the best medicines or combination of medicines for the patient. Since antidepressants often taken several weeks before they are fully effective and side effects begin to lessen, discovering the right treatment calls for patience and good doctor patient communication. Furthermore, ceasing antidepressants abruptly can cause withdrawal symptoms which worsen depression.
Sometimes these medications are given in combinations.
Primary care physicians or psychiatrists many prescribe a number of different medications to a patient to treat different symptoms. These prescriptions may include stimulants, mood-stabilizers, anti-anxiety medications or antipsychotic drugs. In some cases, two or more antidepressants maybe prescribed along with other medications to enhance the effectiveness of the treatment. This strategy is known as augmentation.
Then there’s talk therapy or psychotherapy.
Psychotherapy, usually referred to as “therapy” is generally part of any treatment for depression. It’s probably what most people think of when considering getting help for any emotional problem. Practiced by different types of therapists, it is aimed at assisting the patient to understand what is causing their depression and how to deal with these issues. Often therapy takes place while the patient is also receiving medication to eliminate or lessen the symptoms suffered during depression such as anxiety and insomnia. Through therapy, the patient strives to regain control over his or her emotions and ability to take pleasure in day-to day-activities.
Depending on the cause of the depression, the personality of the patient and other factors, a therapist may try one or more of the following therapy approaches:
- Psychodynamic Therapy
This starts with the assumption that the patient’s depression is caused by unresolved and probably unrecognized difficulties that began in childhood. During the course of therapy, the patient strives to understand these feelings and develop strategies to cope with them. Depending on the patient and the severity of the problem, the course of treatment can take a relatively short period or continue for several years.
- Interpersonal Therapy
As the name implies, this therapeutic approach centers on the interworking of relationships between the patient and their family and friends. The goal is to increase the patient’s self-esteem and improve their ability to communicate with others within a relatively short timeframe of three or four months. It is particularly well suited to treat depression caused by specific events such as a death, the end of a relationship, job loss and other major life events.
- Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy of CBT is based on the premise that by changing a person’s perception of a situation you can alter the way they react to it. So while the situation remains the same, the patient is able to overcome his or her previous feelings of anxiety or depression in response to it.
In contrast to other approaches which focus on analyzing behavior and delving into the patient’s emotional relationships, CBT concentrates on teaching the patient a different way of looking at the world and thus, reacting to it. The therapist acts as an instructor to the patient, guiding them through changing the way he or she thinks, feels, and acts within the context of a particular situation. This type of therapy is appropriate for children as well as adults. By replacing depressing or worrying thoughts, it allows the child to experience feelings that are more appropriate and exhibit more positive behaviors.
Pharmaceutical or psychotherapy – which is best?
Ever since the advent of pharmaceutical treatment for depression, there have been studies touting the benefits of medication for treating depression. Doctor frequently recommend a combination of both medication and therapy for their patients. But recent studies seem to indicate that different patients may benefit more from one of these than another, depending on the root cause of their depression and the physical structure of their brains. Here’s an example of these findings described in a New York Times article, “To Treat Depression, Drugs or Therapy?” by Dr. Richard A. Friedman.
“In a large, multicenter study, Dr. Charles Nemeroff, then a professor of psychiatry at Emory and now at the University of Miami, found that for depressed adults without a history of abuse, there was a clear ranking, order of treatment efficacy: Combined psychotherapy (using a form of cognitive behavior therapy) and an antidepressant (in this case, Serzone) was superior to either treatment alone. But for those who had a history of childhood trauma, the results were strikingly different: 48 percent of these patients achieved remission with psychotherapy alone, but only 33 percent of these patients responded to an antidepressant alone. The combination of psychotherapy and a drug was not significantly better than psychotherapy alone.”
“One explanation for the varying response is that a history of trauma early in life is strongly correlated with shrinkage of the hippocampus, a brain region critical to memory and learning. Perhaps if you are depressed with a compromised hippocampus, you need the active learning that comes with psychotherapy to beat your depression. Antidepressants alone may not suffice.”
Electroconvulsive Therapy (ECT), one of the oldest treatments, is still seen as effective.
Electroconvulsive therapy or ECT has been used to treat depression for decades. Unfortunately, in some cases the treatment was misused and ECT acquired a reputation for harming patients as much as it helped them. Today, however, the American Psychiatric Association has developed strict guidelines for using this procedure and most states require that patients grant their written consent before ECT can be used. In addition, an explanation of the procedure including all the risks involved must be given to the patient and their family before they sign the consent form. Generally, ECT is used only after psychotherapy and medication have proven to be ineffective. Since it works far quicker than medication or therapy, it is also used when there’s an immediate risk of suicide if the depressed state is not relieved.
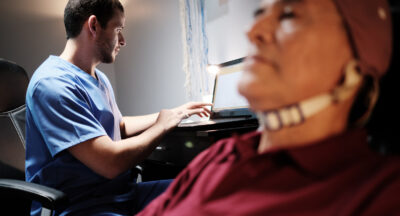
Transcranial Magnetic Stimulation (TMS).
This is a noninvasive therapy used to treat cases of depression, psychosis, anxiety, and other disorders that seem resistant to other forms of treatment. First developed in 1985, its often referred to as rTMS standing for repetitive Transcranial Magnetic Stimulation. The treatment consists of short electromagnetic pulses administered through a coil placed against the scalp near the forehead. These magnetic pulses pass through the skull and cause small electrical currents that stimulate nerve cells in a designated area of the brain.
According to the National Institute of Mental Health, scientists theorize that because TMS focuses on specific sites in the brain, the types of side effects generally associated with ECT are largely eliminated. But opinions still vary as to which site is most effective in treating depression.
There is, of course, one therapy for depression that I have not yet mentioned – Neurofeedback.
However, neurofeedback therapy for depression is too large a topic to be reduced to just a few paragraphs and deserves a discussion all of its own. So join me for part 3 of this series where I’ll examine just why neurofeedback is often more successful than pharmaceutical and talk therapy interventions for treating depression.
Related Posts
How Can I Improve My Anxiety?
Anxiety is a common and often debilitating mental health condition that affects...
How Do I Improve My Executive Functioning?
Executive functioning is a set of mental skills that help us manage time, pay...
The Impact Of COVID-19 On Our Mental Health
The title of this blog post suggests doom and gloom. Yes, we will discuss the...
Attention Deficit Disorder ADD and ADHD Treatment in Chicago: Neurofeedback and Executive Functioning Training
By Ari Goldstein, Ph.D. Most psychologists and doctors in Chicago have limited...