Seasonal Affective Disorder: More than the “Winter Blues”
Seasonal Affective Disorder (SAD)
Seasonal Affective Disorder also known as its acronym SAD, seasonal depression, or winter depression. According to the Diagnostic Manual of Mental Disorders, (DSM-5), is categorized as a form of depression, more specifically Major Depressive Disorder with seasonal Patterns.
This means for many people, SAD begins to occur most often in autumn lasting throughout winter. The reason for this pattern is the general lack of sunlight during these months; because of this, as spring approaches many people find relief from the symptoms of SAD.
Scientists are still working to gain a better understanding of what causes SAD, but let’s explore what they do know.
What causes SAD?
Research indicates that those suffering from SAD may be unable to maintain normal serotonin levels in the brain due to the decrease in sun exposure during the winter months and its shorter hours of daylight. Studies have also shown that people with SAD may have reduced activity of the brain chemical serotonin which is essential in regulating mood. Other findings suggest that those with SAD produce Melatonin in excess. Melatonin is a hormone that serves to regulate and maintain the typical sleep-wake cycle, but when overproduced it can lead to an increase in sleepiness. In addition to the issues that can arise without the typical serotonin production, those with SAD can be prone to Vitamin D deficiency because of the lack of sun exposure. Vitamin D promotes serotonin activity and is commonly absorbed through the skin when exposed to sunlight. So, with shorter days in winter, coupled with cold and dreary weather, those with SAD find themselves short of another source of serotonin production. Without the appropriate production of both melatonin and serotonin, daily rhythms and routines can be disrupted, leading to changes in sleeping habits, mood, and behavior.
Who can have SAD?
Anyone can experience SAD, but it is most prevalent in adults between the ages of 18 and 30 with up to 3% of the general population being affected annually. Among those with major depressive disorder 10-20% will also experience SAD. Millions of Americans have SAD, predominantly affecting women more than men, and is most common with people who live in northern regions that experience shorter days in the winter.
Symptoms of SAD?
An individual experiencing SAD may experience symptoms including but not limited to the following:
- Feelings of sadness
- Depressed mood
- Loss of interest in activities once enjoyed
- Change in appetite
- Change in sleep habits. (one may find themselves sleeping more than usual)
- Increase in restlessness ( not only physically but also mentally)
- Increased fatigue (slowed movements with an intensity observable to others)
- Feelings of worthlessness or guilt
- Thoughts of death or suicide
Common Treatments
There are several ways people commonly seek treatment. Medication, therapy, and an adjustment to routine can assist in the improvement of patients.
Antidepressants can be taken to improve the symptoms that often occur in SAD. These are called SSRIs, Selective serotonin reuptake inhibitors, and are the medication most often prescribed to treat SAD. Because SAD can be exacerbated by the lack of sunlight, taking vitamin D supplements can help restore a healthy balance from the lack of sunlight in the fall and winter months. It is important that you consult with your doctor to discuss how much vitamin D is appropriate for you. Additionally, two omega-3 fatty acids — eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) — are thought to have the most potential to benefit people with mood disorders. There has been a substantial amount of research done that suggests incorporating these acids into your diet can be beneficial. These acids are commonly found in fish oil pills, and doses for depression range from less than 1g/day to 10g/day, but most studies use doses between 1-2g/day.
There are a few types of therapy that often help with SAD, including talk therapies like Cognitive Behavioral Therapy (CBT) or psychotherapy, and light therapy. The patient will consult with a therapist or counselor about current events and feelings in their life, and work together to process those feelings, working to manage them. Light therapy is a unique therapy that requires patients to expose themselves to a therapy light for roughly 20 minutes a day to combat the lack of sunlight that commonly occurs in the fall and winter months. Positive effects can be seen in as little as two weeks. Others might take a more natural approach to sun exposure and increase the time spent outside, but be sure to wear sunscreen! Some other examples include going for more walks, while others may rearrange their living space to be more conducive to receiving natural light.
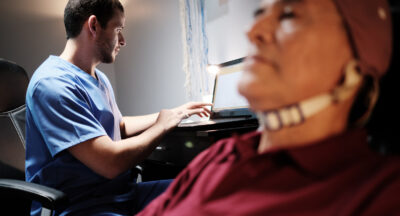
What is Neurofeedback therapy and how can it help?
Neurofeedback is a kind of biofeedback which focuses on retraining the brain by measuring brain wave activity, and providing a feedback signal that clinicians can use to identify common mental health disorders. During neurofeedback therapy sessions, audio and/or video signal cues are actively relayed to the patient, offering positive or negative feedback responses for desirable or undesirable brain wave activity. This unique therapy can help the patient better understand the direct and immediate impact their training is having on their brain, while actively retraining the brain in the process. There are multiple brain waves that could create SAD symptomatology, and through a qEEG (Quantitative Electroencephalogram) clinicians are able to determine the imbalance, and what treatment protocols will be best for the patient. The most common protocol for SAD is alpha-theta training, though some clients may need more attention on beta waves; alpha-theta training has shown a tremendous amount of promise for patients starting neurofeedback therapy programs, after more traditional therapies were ineffective at treating SAD. Neurofeedback therapy has also become an alternative form of treatment for patients that suffer from Treatment-Resistant Depression (TRD), along with many other forms of depression. Neurofeedback therapy has also shown to be effective at reducing symptoms often seen with other common mental health disorders.
If you or someone you know is suffering from Seasonal Affective Disorder be sure to consult your doctor or a trained medical professional for guidance before participating in these forms of treatment.
Cognitive Solutions LC works with individuals suffering from SAD through psychotherapy and neurofeedback. For more information about our treatments and teletherapy options, please contact us at (773) 755-1775 or email info@helpforld.com.
References
- American Psychiatric Association. Seasonal Affective Disorder 2020.
- The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5); American Psychiatric Association.
- Lee YJ, Lee GW, Seo WS, Koo BH, Kim HG, Cheon EJ. Neurofeedback Treatment on Depressive Symptoms and Functional Recovery in Treatment-Resistant Patients with Major Depressive Disorder: an Open-Label Pilot Study. J Korean Med Sci. 2019 Nov 4;34(42):e287. doi: 10.3346/jkms.2019.34.e287. PMID: 31674161; PMCID: PMC6823520.
- Marzbani H, Marateb HR, Mansourian M. Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications. Basic Clin Neurosci. 2016 Apr;7(2):143-58. doi: 10.15412/J.BCN.03070208. PMID: 27303609; PMCID: PMC4892319.
- Mischoulon, David. Omega-3 Fatty Acids for Mood Disorders. 2020, Oct 27. https://www.health.harvard.edu/blog/omega-3-fatty-acids-for-mood-disorders-2018080314414
- U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health.
Related Posts
The History of Neurofeedback: Part I
How does Neurofeedback work? Why is it so effective in treating brain conditions...
Adult Attention Deficit Hyperactivity Disorder
Adult attention deficit hyperactivity disorder (ADD or ADHD) manifests itself...
Attention Deficit Disorder ADD and ADHD Treatment in Chicago: Neurofeedback and Executive Functioning Training
By Ari Goldstein, Ph.D. Most psychologists and doctors in Chicago have limited...
Back-to-School Checklist — Why You Should Consider a Private Tutor
At Cognitive Solutions L.C., we understand the unique challenges that students...